Over 7 percent of U.S. adults had a major depressive episode last year. This shows how common mood disorders are, especially major depressive disorder (MDD) and persistent depressive disorder (PDD) or dysthymia. About 2.5 percent of people will face PDD at some point, showing the need to understand these issues.
MDD and dysthymia have similar symptoms, but they vary in severity and how long they last. Major depression has intense symptoms lasting at least 2 weeks. Dysthymia’s symptoms are milder but go on for at least 2 years. Knowing the difference is key for the right help and support.
These disorders affect more than just emotional health. They influence overall well-being and everyday life. To learn how dysthymia is different from major depression and the treatments for each, read the insights in this article. For more details, visit this link.
Key Takeaways
- Over 7% of adults in the U.S. will experience a major depressive episode annually.
- Approximately 1.5% of adults are affected by persistent depressive disorder during their lifetime.
- Understanding the duration and severity of symptoms is essential for diagnosis.
- Common treatment options include medication and therapy tailored for each condition.
- Most individuals with PDD may experience episodes of major depression, leading to “double depression.”
- Females are more commonly diagnosed with both MDD and PDD throughout their lives.
Understanding Dysthymia and Major Depression
Persistent depressive disorder and major depression differ, yet both are mood disorders. In the US, 17% suffer from major depression. In contrast, 3% experience persistent depressive disorder. Even though those with persistent depressive disorder show fewer symptoms, these can last over two years.
Those with persistent depressive disorder may also face major depression, a scenario called double depression. This situation shows how complex these mental health issues are. It’s important to know that depression hits women twice as often as men. This fact stresses the importance of quick help and awareness.
Many factors trigger these conditions, including genetics, trauma, and self-esteem issues. Noticing changes in eating habits and weight can signal the difference between the two. Persistent depressive disorder doesn’t discriminate. It can affect anyone, regardless of age or background. Studies show about 11% of youths 13 to 18 years old face these disorders.
Knowing about persistent depressive disorder and major depression helps. Their symptoms often mix, making diagnosis hard. Clear definitions are key. They help people realize these are serious issues that go beyond just bad days.
What is Dysthymia?
Dysthymia, or persistent depressive disorder, is a long-term form of depression. It’s marked by constant low feelings lasting a long time. For adults, symptoms must last at least two years. For kids and teens, it’s one year. Many people miss the signs of dysthymia. This can lead to ongoing discomfort and affects daily life.
Definition of Persistent Depressive Disorder
Persistent depressive disorder, or dysthymia, is chronic, mild depression. It leads to long-term sadness. People with dysthymia struggle to feel joy or satisfaction. Because it’s persistent, symptoms often go unnoticed for years. About 75% of dysthymia patients may have a major depressive episode. This shows why it’s vital to recognize and treat it properly.
Symptoms of Dysthymia
Symptoms of dysthymia differ from major depression. Key signs include:
- Prolonged feelings of sadness or emptiness
- Fatigue or low energy
- Low self-esteem
- Difficulty concentrating or making decisions
- Changes in appetite or sleep patterns
These symptoms often affect individuals regularly. This can harm their emotional wellbeing. It can also impact personal and work relationships. Getting help early is key. Proper care helps recovery through therapy and medication.
What is Major Depression?
Major depression is a significant mental health issue. It is different from other types of depression like dysthymia. This is because of its severe episodes. Knowing what it is and its symptoms helps understand how it affects lives.
Definition of Major Depressive Disorder
Major depressive disorder has five or more symptoms over two weeks. These include deep sadness, losing interest in fun activities, weight changes, and trouble sleeping. It also includes feeling very tired, worthless, and having trouble thinking. Spotting these signs is key. They can mess up daily life and have long-lasting effects if ignored.
Symptoms of Major Depression
- Deep feelings of sadness or emptiness
- Loss of interest in previously enjoyed activities
- Significant weight loss or gain without dieting
- Insomnia or hypersomnia
- Feeling fatigued or lacking energy
- Feelings of worthlessness or excessive guilt
- Difficulties concentrating or making decisions
- Thoughts of death or suicide
Every year, major depression impacts 5% to 10% of adults in the U.S. This problem often comes back. Up to half might face another episode within a year after the first. Knowing the early signs is crucial. It leads to getting the right help.
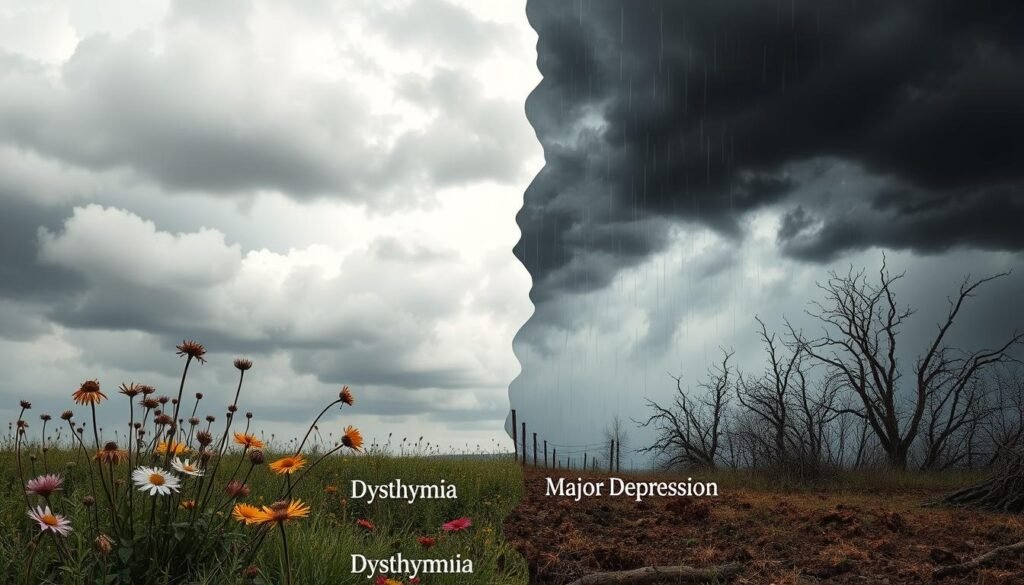
How Dysthymia Differs from Major Depression
It’s important to know how dysthymia is different from major depression for those dealing with mood issues. Dysthymia, or Persistent Depressive Disorder, means being in a low mood for at least two years. The symptoms are milder but last longer, giving little relief. On the flip side, major depression has stronger symptoms but for short periods. For a diagnosis of major depression, one needs at least five symptoms lasting over two weeks.
Both conditions affect everyday life greatly. People with major depression see a big change in their daily routines because of symptom severity. These symptoms can be very tough, even leading to thoughts of suicide that need quick help. However, those with dysthymia deal with ongoing low energy, sadness, and a drop in interest. Their symptoms aren’t as severe as those seen in major depression.
The numbers show interesting trends. Dysthymia hits women twice as much as men, calling for targeted mental health help. While dysthymia needs symptoms to last two years, major depression’s episodes are brief yet intense. Both require a careful diagnosis and action plan.
| Feature | Dysthymia | Major Depression |
|---|---|---|
| Duration of Symptoms | At least 2 years | At least 2 weeks |
| Severity of Symptoms | Less severe but persistent | Severe and debilitating |
| Episodic Nature | Chronic and continuous | Shorter episodes |
| Risk of Suicide | Less common | More prevalent |
| Gender Disparity | More common in women | Varies |
Understanding the differences between these mood disorders helps lead to better mental health care. It’s crucial for finding the right way to help those affected.
Duration of Symptoms in Dysthymia vs Major Depression
Symptom duration is key in telling apart chronic depression from major depressive episodes. Knowing how long and how persistently each condition affects someone helps us understand them better.
Chronic Nature of Dysthymia
Dysthymia, now called persistent depressive disorder, lasts a long time. People with it face symptoms for over two years, making it hard to pinpoint when it started. This long-term struggle means many get used to their sadness, which impacts daily life and happiness.
Episodes of Major Depression
Major depressive episodes, on the other hand, last at least two weeks. But, they can happen again and again over someone’s life. Each episode brings a noticeable decline in mood and ability to function. This shows the difference between ongoing depression and times of deep sadness.
| Aspect | Dysthymia (Persistent Depressive Disorder) | Major Depression (MDD) |
|---|---|---|
| Duration of Symptoms | More than two years | Minimum of two weeks |
| Onset | Typically starts in adolescence | Averages around 40 years old |
| Frequency | Constant, may vary in intensity | Episodic, can occur multiple times |
| Impact on Life | Consistent emotional challenges, lower quality of life | Impact varies based on individual episodes |
Impacts on Daily Life
Both dysthymia and major depression deeply affect how a person functions daily. Knowing about these impacts helps us understand their effects on everyday life.
Effects of Dysthymia on Daily Functioning
Dysthymia is a long-term form of depression. It makes people feel sad for two years or more. People with dysthymia often feel too tired or unmotivated to do their daily tasks well.
They might keep up with some activities, but work and relationships usually suffer. Over time, they might stop doing things they once enjoyed.
Effects of Major Depression on Daily Functioning
Major depressive disorder, or MDD, causes severe symptoms that quickly affect daily life. These intense episodes last for weeks. They can make people miss work or lose interest in social activities.
People may start to pull away from loved ones, hurting their emotional health. The serious impact of depression makes finding a good treatment very important.
Common Risk Factors for Both Conditions
It’s crucial to know the common risk factors for depression. This includes looking at dysthymia and major depression. We need to consider genetics, environment, and social issues. These factors can lead to mental health problems.
Genetic Vulnerability
Genetics are key in dysthymia and major depression. If depression runs in your family, you’re more at risk. In fact, genes can play a 30-40% role in your chance of getting depressed. Knowing your family’s health history helps in understanding your own risks.
Life Events and Stress
Difficult times and chronic stress can start major depression and dysthymia. Stressful events might make things worse for people already at risk. Things like long-term illness and drug problems increase this risk. So, grasping how stress affects you is critical. It helps doctors and patients plan better treatments.
| Risk Factor | Dysthymia | Major Depression |
|---|---|---|
| Family History | Yes | Yes |
| Chronic Stress | High | High |
| Traumatic Events | Possible Trigger | Common Trigger |
| Substance Abuse | Linked | Linked |
| Chronic Illness | Contributory Factor | Contributory Factor |
For more information on depression, check out this resource.
Treatment Options for Dysthymia and Major Depression
Treatment for dysthymia and major depression often includes different methods. These methods can be psychotherapy and medication, fit to the person’s needs. Knowing about these options is key for better managing symptoms and improving well-being.
Therapeutic Approaches
Psychotherapy is crucial in treating depression. Cognitive Behavioral Therapy (CBT) is a top method for managing major depression. It helps people change negative thoughts and find coping strategies. Other methods like talk therapy help patients deal with crises and life changes. Activities like journaling and reading self-help books also help build emotional strength.
Medication Management
Medication often includes antidepressants to adjust the brain’s chemical balance. There are many antidepressants, like SSRIs and SNRIs, used often. Finding the right medication sometimes means trying several options. It’s important to know about side effects, like the U.S. FDA warning of increased suicide risk in young people, for safe treatment.
| Treatment Type | Description | Examples |
|---|---|---|
| Psychotherapy | Talk-based therapies aimed at improving mental health. | Cognitive Behavioral Therapy, Talk Therapy |
| Medication | Pharmaceutical treatments to alleviate depression symptoms. | SSRIs, SNRIs, Tricyclic Antidepressants |
| Alternative Therapies | Complementary methods to enhance traditional treatment. | St. John’s Wort, relaxation techniques |
| Self-Care | Strategies individuals can implement to improve well-being. | Regular exercise, healthy diet, avoiding substances |
Combining psychotherapy, medication, and self-care strategies helps manage depression effectively. Knowing about treatment options helps patients and supports their recovery journey. For more information, see this resource on depression treatments.
Double Depression: A Combination of Both Disorders
Double depression is when someone has both persistent depressive disorder (PDD) and major depressive disorder (MDD). This condition makes emotional health harder as symptoms from each disorder make things worse. PDD needs symptoms to last for two years while MDD symptoms should be present for at least two weeks.
The DSM-5-TR doesn’t list double depression as its own diagnosis. Yet, individuals with this condition often suffer more intense symptoms. PDD symptoms can include eating and sleeping problems, feeling really down about oneself, and always feeling hopeless. MDD symptoms can involve feeling extremely sad, very tired, and thinking about self-harm a lot.
Treating double depression involves therapy, medication, and changing some life habits. Types of therapy like cognitive behavioral therapy (CBT) and dialectical behavioral therapy help with symptom relief. Doctors might prescribe medications like SSRIs and SNRIs, which take time to work. So, patients need to stay in touch with their doctors.
Making lifestyle changes also helps with symptom management. Eating better and exercising more can make a big difference. It’s common for people with dysthymic disorder to go through major depressive episodes. Proper treatment planning is key in helping those with double depression. Check out this detailed source for more information.
Mental Health Implications of Dysthymia and Major Depression
Dysthymia (PDD) and major depression deeply affect mental and physical health. PDD can last for years, causing long-term low moods. Recognizing these conditions’ effects helps manage and treat them properly.
Impact on Emotional Wellbeing
Those with PDD and major depression often struggle emotionally. They might feel hopeless, think less of themselves, or sleep poorly. Additionally, PDD can lead to major depressive episodes, worsening emotional pain.
PDD also raises anxiety levels, making it hard for people to cope. Early help and thorough treatment are key to improving lives.
Long-term Health Effects
Depression doesn’t just affect the mind; it can harm the body too. Chronic depression, like PDD, raises the risk of heart problems. Neglecting personal care may result in obesity, high blood pressure, or diabetes.
This shows how critical proper treatment is for those with PDD and major depression. By getting help regularly, people can live better and healthier.
| Condition | Emotional Wellbeing Impact | Long-term Health Risks |
|---|---|---|
| Persistent Depressive Disorder (PDD) | Chronic low mood, anxiety, low self-esteem | Cardiovascular issues, substance abuse, neglect of self-care |
| Major Depression | Severe episodes of low mood, hopelessness | Potential physical health problems, increased suicide risk |
Both patients and doctors need to understand these disorders well. For more about PDD, check out this resource.
Conclusion
Dysthymia and major depression are two conditions with important differences and similarities. These differences are key in treating and managing them. Dysthymia is a long-term, low mood lasting for years. But major depression has more intense symptoms that come and go. Knowing how both affect daily life is crucial for the right therapy.
It’s vital to understand the negative beliefs and behaviors behind these conditions. People with dysthymia often face lasting negative thoughts that keep the depression going. Tackling these thoughts with therapy can help improve their mood and prevent more episodes.
There is hope for those dealing with dysthymia through effective treatments. Although many receive help, more work is needed to ensure care is the best it can be. With the right support, people can start to heal. This leads to a better life and a hopeful future.