Did you know that nearly three in ten adults—29%—have faced depression? This shocking number shows how common this mental health problem is. It also shows why we must deeply understand depression anatomy. In the U.S., about 17.3 million adults deal with depression yearly, which affects their daily life and happiness.
This guide dives into what depression anatomy means, looking at all its parts. We look at the brain reasons behind depression to better understand it. This article points out how complex depression is as a mental health issue. Knowing more helps people deal with depression’s challenges. This knowledge guides them toward effective healing and getting better.
Key Takeaways
- Depression affects nearly 29% of adults at some point in their lives.
- The condition impacts approximately 17.3 million adults in the U.S. each year.
- Understanding depression anatomy helps in recognizing its complexities.
- Knowledge about depression pathways can lead to better treatment outcomes.
- Increased awareness can foster a supportive environment for those affected.
Understanding Depression
Depression is not just feeling sad. It’s a serious mood disorder that changes how you feel, think, and handle daily activities. The definition of depression includes many signs, like feeling sad often or losing interest in things you once loved. About 6% of U.S. adults had a major depressive episode in 2020, showing how widespread it is.
Depression’s key signs are not only about being sad. They also involve big changes in how much you eat or sleep, and how well you can focus. You might feel very tired all the time, lose your motivation, and feel helpless. These feelings need to last at least two weeks to be considered major depressive disorder.
Chronic stress plays a big role in causing depression. It causes complex changes in the brain’s activity. Studies found that in depressed people, the amygdala gets overactive, especially when seeing sad faces. This overactivity can make emotional distress worse.
The nucleus accumbens, important for feeling rewards, works less in those who are depressed. This can make it hard to feel happy or pleased. Studies with animals found they need bigger rewards to feel happy when stressed, much like humans with depression.
Understanding depression is key in finding the right treatments to get better. As we learn more about depression, it’s crucial to know both the mental and physical aspects of this disorder. It helps in treating and supporting those affected.
Depression Anatomy Definition
To grasp depression, we must look at its many sides. The depression anatomy definition covers the mind aspects and the body and brain parts that play a role in this complex issue. It’s deeper than just feeling sad. It involves intense symptoms that disrupt daily life and happiness. Knowing the difference between simple sadness and clinical depression is key for those seeking support.
Overview of Depression
Depression affects a person’s thoughts, emotions, and actions in different ways. It brings on lasting feelings of despair, a drop in interest in once-loved activities, and focus problems. It’s important to know the types of depression well. This knowledge is crucial for creating good treatment plans, as each type is unique with its own features and triggers.
Types of Depression
There are several kinds of depression, each needing its own way of care and handling. Recognized types of depression are:
- Major Depressive Disorder: Shows through deep sadness spells, messing with everyday life.
- Persistent Depressive Disorder (Dysthymia): A long-term depression kind, marked by ongoing low mood.
- Perinatal Depression: Happens during pregnancy or after having a baby, affecting new moms.
- Seasonal Affective Disorder (SAD): Connected to season shifts, often due to less sunlight.
- Depression with Psychotic Features: Comes with intense depression plus hallucinations or false beliefs.
Each depression type calls for a unique treatment plan, stressing the need for expert advice in handling these deep issues. For those wanting to know more about how our bodies move, you can get a better idea by looking at this resource.

| Type of Depression | Characteristics | Common Symptoms |
|---|---|---|
| Major Depressive Disorder | Intense episodes disrupting daily life | Sadness, fatigue, loss of interest |
| Persistent Depressive Disorder | Chronic low mood lasting for years | Pessimism, fatigue, hopelessness |
| Perinatal Depression | Occurs during or after pregnancy | Sadness, anxiety, changes in sleep |
| Seasonal Affective Disorder | Triggered by seasonal changes | Fatigue, weight gain, social withdrawal |
| Depression with Psychotic Features | Severe depression with hallucinations | Delusions, confusion, severe mood changes |
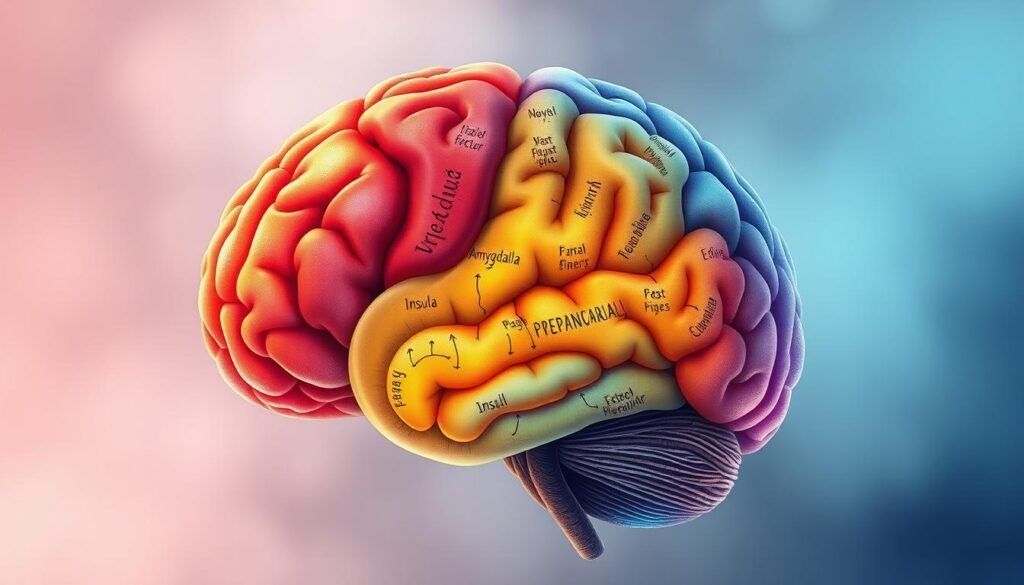
Brain Regions Involved in Depression
Grasping how depression works means understanding its effects on the brain. The brain has areas that handle our emotions and decisions. The amygdala and prefrontal cortex play big roles in depression, showing its complexity.
Role of the Amygdala
The amygdala helps us process and react to emotions. When it’s more active, people feel more fear and sadness, a common trait in depression. Studies show changes in the amygdala in depressed individuals, such as reacting more to sad things. It also affects how we remember emotions and view social interactions.
Importance of the Prefrontal Cortex
The prefrontal cortex is key for mood control and thinking. In depression, this area can change, making it hard to make decisions or focus. Less activity in parts of the cortex is linked with feeling depressed. These brain changes can make depression tougher to manage.
Neurological Basis of Depression
The neurological basis of depression is complex and involves many factors. It’s about how various brain chemicals interact and how the brain’s structure can change. Understanding these aspects is vital to know how depression appears and impacts people.
Neurotransmitters and Their Impact
Neurotransmitters like serotonin, dopamine, and norepinephrine play a key role in mood regulation. An imbalance in these substances often leads to depression. The monoamine hypothesis, for example, explains how shortages in these neurotransmitters can trigger depressive symptoms. Studies have shown changes in serotonin activity in those with depression, highlighting the disorder’s biochemical roots.
Structural Brain Changes in Depression
Studies show that people with major depressive disorder may see changes in their brain structures. Important areas like the hippocampus and prefrontal cortex, which govern emotions and thinking, can change. These changes can reduce brain size and affect how brain areas connect. This shows the significant effect depression has on the brain’s form.
Neuroimaging studies back up the idea that these structural changes are common in depression. This information supports early intervention and thorough treatment strategies. It’s crucial for tackling the neurological elements of depression.

| Neurotransmitter | Impact on Depression |
|---|---|
| Serotonin | Regulates mood and emotional well-being; low levels linked to depression. |
| Dopamine | Involved in reward and pleasure; dysregulation can lead to depressive symptoms. |
| Norepinephrine | Affects attention and responding actions in the brain; imbalances can exacerbate depressive episodes. |
For more info on depression’s neurological side, check out this article and guides on getting help for depression.
Depression and the Hippocampus
Depression and the hippocampus are closely linked, affecting memory and thinking. The hippocampus is crucial for learning, forming memories, and handling emotions. Studies have found that long-lasting depression can shrink the hippocampus, which hurts memory and mood.
Research on people who have passed away shows few dead cells in the hippocampus of those who were depressed. This hints that other factors are involved. High stress hormone levels in depression may block new nerve growth. This can lead to issues with memory, as found in tests.
One study found that stress can lead to a smaller hippocampus. It also found changes in brain areas that control mood. These changes may include shrinking nerve connections and losing supportive brain cells. This makes depression and memory problems more complex.
Studies on animals show that antidepressants can help grow new nerve cells in the hippocampus. They also increase a brain growth chemical. This suggests that treating depression early might not only lift mood but also prevent brain damage affecting thought and memory.
| Impact of Depression on the Hippocampus | Effect on Memory |
|---|---|
| Volume Reduction | Impaired recall and recognition |
| Increased Glucocorticoids | Stress-related cognitive dysfunction |
| Cellular Changes | Memory problems and concentration difficulties |
| Neurogenesis Decrease | Long-term memory issues |
| Cortical Damage | Emotional instability and executive dysfunction |
Understanding how depression affects the hippocampus can lead to better treatments. Early treatment might help save memory and thinking skills.
Depression and the Amygdala’s Role
The amygdala plays a crucial role in how we handle emotions. It is especially important for understanding depression. When the amygdala is more active, it changes how we regulate our emotions. People with depression often see their amygdala light up more, making them extra sensitive to feelings.
This increased sensitivity can lead to ongoing sadness and quick irritability. This is common in those with major depression. By looking into the amygdala’s function, researchers learn more about its ties to our emotions and thoughts. An imbalance in this area can lead to mood swings, anxiety, and lacking joy in activities once enjoyed.
Below is a simple table that shows how the amygdala affects emotions and its link to depression:
| Aspect | Amygdala Activity in Depression | Emotional Regulation Implications |
|---|---|---|
| Heightened Activation | Increased emotional sensitivity | Leads to persistent sadness |
| Persistent Reactions | Amplified feelings of irritability | Struggles with emotional balance |
| Connection to Other Disorders | Common in PTSD and anxiety | Reinforces emotional dysregulation |
The amygdala’s involvement offers key insights into better treatments. Knowing more helps create effective ways to support those dealing with these emotional challenges.
Neuroimaging Studies of Depression
Neuroimaging studies have become key in understanding depression’s deep-seated brain-related causes. Every year, experts publish over 250 new articles in places like PubMed. These studies aim to find what makes those with Major Depressive Disorder (MDD) different from people without mental health issues.
Key Findings from Neuroimaging Research
MRI scans show changes in brain areas dealing with emotions in those with MDD. Techniques like voxel-based methods identify crucial areas. The anterior cingulate cortex, medial prefrontal cortex, and amygdala are among them. PET scans help us understand how these people’s brains deal with feelings and rewards.
One finding is more activity in brain areas linked to emotions when faced with sad or stressful things. Also, people with bigger hippocampal areas tend to respond better to treatment. This implies that some brain changes can predict therapy success.
Yet, pinpointing exact brain activity changes in depression is hard. The quest includes separating depression from other conditions like anxiety. But, advancing neuroimaging research could lead to better ways to diagnose and treat depression. For more info, check out numerous detailed studies here.
Neurocircuitry of Depression
The neurocircuitry of depression shows how our brain areas work together. They help control our moods, feelings, and thoughts. This network is key in diagnosing and treating depression. By studying these brain connections, we can find better ways to help those with major depression.
Many studies focus on parts of the brain like the reward system and the amygdala. They show how these areas affect our emotions and decisions. Also, learning about how our brain circuits develop helps us understand mental disorders better. With over 405 million people worldwide dealing with depression, researching these brain networks is very important. It can lead to better treatments, especially ones based on neuroimaging studies.
New scanning technologies are giving us deeper insights into depression. They show us how certain brain connections aren’t working as they should. Scientists have found six main circuits linked to depression and anxiety. Learning about these networks can help improve mental health. It opens up possibilities for new and better treatments.