Almost 85% of people think that depression is mainly due to brain chemistry issues. Neurotransmitters are crucial for our mental well-being. They regulate how we feel emotionally.
But the idea that just chemical imbalances cause depression is outdated. A 2023 study in Molecular Psychiatry showed many factors contribute to depression. These include our genes, environment, and how we see the world. Serotonin, dopamine, and norepinephrine play important roles, but they’re part of a bigger picture.
It is key to grasp these complex factors. Understanding the role of neurotransmitters in depression can lead to better treatments. It helps those with depression and professionals aiming to support them.
Key Takeaways
- 85% of people attribute depression to chemical imbalances in the brain.
- Neurotransmitters like serotonin, dopamine, and norepinephrine are central to mood regulation.
- Recent research suggests the causes of depression are more complex than simple neurotransmitter imbalances.
- Genetics and psychosocial factors play a significant role in the onset of depression.
- Understanding neurotransmitter roles can improve treatment strategies for depression.
Understanding Depression: A Complex Mental Health Condition
Depression is a complex mental health issue that impacts people worldwide. It’s marked by ongoing sadness, a lack of interest in activities, and difficulties in everyday life. Recognizing its complexity is vital, as Major depressive disorder (MDD) is a leading cause of disability globally. Unfortunately, many with MDD don’t get the help they need, making life even more challenging.
The causes of depression vary greatly. Genetics play a role in 30-40% of cases, showing that inheritance matters. The remaining 60-70% comes from factors like tough childhoods and relationship problems. Notably, women often face more stress, which may explain their higher rates of depression.
Depression can also harm physical health. High cortisol levels can lead to serious conditions, including heart disease and diabetes. Those with childhood trauma may face even more risk. Their bodies’ stress responses are more likely to be out of balance. This shows how early hardships are linked to later health issues.
Neurotransmitter imbalances are key in mood disorders as well. Low serotonin is linked to depression, and dopamine affects memory and behavior. This mix of genetic, environmental, and psychological factors makes depression complex. It affects everyone differently, significantly impacting their lives.
| Factor | Contribution to Depression |
|---|---|
| Genetic Factors | 30-40% |
| Non-Genetic Factors | 60-70% |
| Impact of Childhood Abuse | Contributes to abnormal HPA axis function |
| Stress Responsiveness | Higher in women |
| Physical Consequences | Increased risk for various diseases |
Neurotransmitters: The Brain’s Chemical Messengers
Neurotransmitters are key chemicals in our brain. They help send signals between neurons. This affects our mood, behavior, and how we handle emotions. Important neurotransmitters like serotonin, dopamine, and norepinephrine keep our mental health stable. When these chemicals are off-balance, our psychological health is impacted.
The theory of chemical imbalance links conditions like depression to changes in neurotransmitter levels. Antidepressant meds work by increasing levels of these chemicals, easing depression. This has led to a better understanding of the role neurotransmitters play in emotional disorders.
Studies show neurotransmitter imbalances can happen in the limbic system. This area is key for handling emotions. Changes here can lead to more anxiety and depression symptoms. For example, having less serotonin can cause emotional problems. This shows how crucial it is to keep these chemicals balanced.
By diving into these processes, new treatments focusing on neurotransmitter function are developed. This helps in supporting mental wellness. As research grows, we learn more about how these chemical messengers play a role in our mental health. For more details on neurotransmitters, click here.
| Neurotransmitter | Function | Effect of Imbalance |
|---|---|---|
| Serotonin | Regulates mood, behavior, sleep, and memory | Depression, anxiety, changes in appetite |
| Dopamine | Influences pleasure, movement, and motivation | Lack of pleasure, depression, irritability |
| Norepinephrine | Involved in stress response and energy regulation | Low mood, fatigue, anxiety, concentration issues |
Key Neurotransmitters Linked to Depression
Understanding the main neurotransmitters linked to depression helps us see the biological side of mental health. These include serotonin, dopamine, and norepinephrine. Each one has a big role in controlling our mood and feelings. When these chemicals are off-balance, it can really impact a person’s mind, sometimes leading to depression.
Serotonin: The “Feel Good” Chemical
Serotonin is known as the “feel good” chemical because it helps control our mood. If serotonin levels are low, people may feel more depressed. This supports the serotonin hypothesis. So, it’s very important for keeping our emotions stable.
Dopamine: The Reward and Pleasure Neurotransmitter
Dopamine is all about reward and feeling good. If we don’t have enough dopamine, we might not enjoy things. This feeling, or lack of it, is a symptom of depression. Dopamine is key to feeling motivated and happy with daily life.
Norepinephrine: The Stress Response Indicator
Norepinephrine deals with how we respond to stress. It’s also important for mood. A theory called the catecholamine hypothesis links it to mood issues. So, it plays a big role in depression by affecting our stress and mood.
Neurotransmitter Imbalances and Their Impact on Depression
Neurotransmitter imbalances play a big role in mood disorders, especially depression. Knowing how these imbalances impact mental health helps in finding the right treatments. Recent studies show a strong link between neurotransmitter imbalances and depression’s intensity and duration.
How Imbalances Contribute to Mood Disorders
About 20% of people worldwide will face a major depressive disorder once in their life. In the U.S., around 14.8 million adults struggle with a major depressive episode every year. This impacts their daily lives. Serotonin, dopamine, and norepinephrine are crucial for mood and emotional well-being.
Several things can cause neurotransmitter imbalances, like genes, poor nutrition, lifestyle, stress, and environmental factors. Nutrients such as B-vitamins, Vitamin C, Vitamin D, and Omega-3 fatty acids are important. They help produce and manage neurotransmitters, affecting treatment results.
Evidence from Recent Research Studies
Studies show not getting enough sleep changes how neurotransmitters work. It affects chemicals like serotonin and dopamine. Trying out mind-body therapies like yoga and meditation can help. They manage imbalances, anxiety, and depression. Exercise also helps by releasing neurotransmitters like dopamine and endorphins. It also increases brain oxygen, helping with norepinephrine imbalance.
It’s important to have personalized treatment plans. This is because 30% to 40% of patients don’t get better with common antidepressants, like SSRIs. Statistics reveal that people with low serotonin activity in the brain are more likely to attempt suicide. With about two-thirds of suicide cases showing signs of depression, it’s vital to focus on neurotransmitter imbalances. Learning about these complex interactions is key for targeted treatments.
| Neurotransmitter | Role in Mood Regulation | Common Causes of Imbalance |
|---|---|---|
| Serotonin | Regulates mood, anxiety, and happiness | Nutritional deficiencies, stress, and lack of sleep |
| Dopamine | Affects pleasure, motivation, and reward | Genetic factors, lifestyle choices, and stress |
| Norepinephrine | Involved in arousal and alertness | Chronic stress, sleep disturbances, and environmental factors |
Environmental and Biological Factors Influencing Neurotransmitter Levels
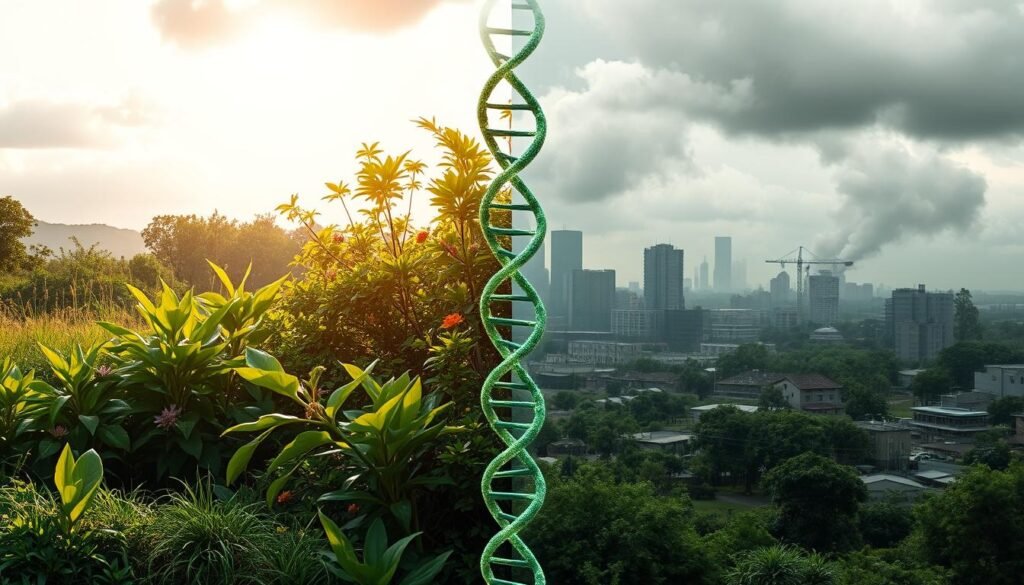
Depression’s complexity comes from both environmental and biological elements. Genetics play a crucial role. However, stress from our surroundings also impacts our mental health. These factors together shed light on depression’s complex nature.
The Role of Genetics in Depression
Genes significantly affect the risk of major depressive disorder (MDD). Studies show that genetics account for 30-50% of MDD cases. There are over 200 genes tied to how our brain chemicals function. When specific genes are not transcribed correctly, it can lead to MDD, emphasizing the role of our biological inheritance.
The Impact of Psychosocial Stressors
Experiencing trauma, ongoing stress, and low support can alter our brain chemistry. These situations make depression symptoms worse and can influence genetic vulnerability. Key brain chemicals like GABA, serotonin, and norepinephrine are affected by stress. This connection underlines the effect of our environment on our mental health.
| Factor | Type | Impact on Depression |
|---|---|---|
| Genetic Predisposition | Biological | 30-50% risk of developing MDD linked to family history |
| Trauma | Environmental | Increases vulnerability to depressive symptoms |
| Chronic Stress | Environmental | Can lead to dysregulation of neurotransmitters |
| Social Support | Environmental | Low social support correlates with heightened depression symptoms |
| GABA Levels | Biological | Lower levels linked to depression |
To understand depression, we must look at genetic factors and life stresses. Acknowledging both offers a full view of how brain chemistry changes, beneficial for mental health care.
The Role of Antidepressants in Managing Neurotransmitter Levels
Antidepressants help balance neurotransmitter levels in the brain. This balance is key for people dealing with depression. Knowing how these medications work is vital for choosing the best treatment.
SSRIs and Their Mechanism of Action
SSRIs are a common choice for treating depression. They increase the brain’s serotonin levels by blocking its reabsorption. This boosts mood and helps lessen depression’s impact. Usually, patients start feeling better within 1 to 4 weeks of starting SSRIs.
Popular SSRIs include Citalopram, Escitalopram, Fluvoxamine, Fluoxetine, Paroxetine, and Sertraline. Each person may react differently to various SSRIs. According to research, they generally have fewer side effects compared to older drugs.
Other Classes of Antidepressants
Other antidepressants are SNRIs, TCAs, and MAOIs. SNRIs target serotonin and norepinephrine. They work differently in each person, affecting how well they treat depression. SNRIs like Desvenlafaxine (Pristiq), Duloxetine (Cymbalta), Levomilnacipran (Fetzima), and Venlafaxine (Effexor XR) are common examples.
SNRIs are good for depression and can also help with anxiety disorders and chronic pain. Understanding different antidepressants helps find the right treatment for depression. The choice often depends on personal health history and specific symptoms.
| Class of Antidepressant | Mechanism of Action | Common Examples | Potential Side Effects |
|---|---|---|---|
| SSRIs | Blocks reabsorption of serotonin | Citalopram, Fluoxetine | Less adverse effects, sexual dysfunction |
| SNRIs | Blocks reabsorption of serotonin and norepinephrine | Duloxetine, Venlafaxine | Nausea, headache, potential blood pressure increase |
| TCAs | Blocks reabsorption of neurotransmitters such as norepinephrine and serotonin | Amitriptyline, Nortriptyline | Weight gain, dry mouth, dizziness |
| MAOIs | Inhibits monoamine oxidase, increasing neurotransmitter levels | Phenelzine, Tranylcypromine | Dietary restrictions required, risk of hypertensive crisis |
Emerging Theories on Depression Beyond Chemical Imbalances
Previously, most people thought depression came from chemical imbalances in the brain. Now, studies suggest the causes of depression are more complex. We need to look at depression using the biopsychosocial model. This approach considers biological, psychological, and social factors in mental health.
Still, over 80% of people believe chemical imbalances cause depression, showing how popular this old idea is. However, even with medication and therapy, only 46% fully recover. This shows we need to look beyond just brain chemicals to help everyone.
Recent research highlights how our lifestyle choices can influence depression risk. A study from Harvard found that exercise can help fight off depression, even for those genetically at risk. Also, ongoing low-grade inflammation is now linked to a higher depression risk. This shows how our environment and actions impact our mental health.
Eating well also matters for our mental well-being. Foods like seafood, leafy greens, and cruciferous vegetables support a healthy mind. Understanding the brain’s vast network, with its trillions of synapses, is crucial in tackling mental health issues.
Looking ahead, we see the need for an integrated depression treatment method. This includes studying how genes and environment affect our brains. By focusing on the biopsychosocial model, we can find better ways to manage depression effectively.
Personalized Approaches to Depression Treatment
Depression treatment must be unique to each person. It’s crucial because everyone has different body chemistry and life experiences. This need for personalized care is supported by research. It shows that people react differently to treatments.
Esketamine represents a breakthrough in depression treatment. It’s the first of its kind approved by the FDA for those who haven’t found other treatments helpful. It quickly helps reduce depression symptoms and is safe for many, including teens and the elderly.
Lifestyle changes can also play a big role in treating depression. For example, what we eat and our gut health can affect our mood. Older adults who took probiotics saw mood improvements. This shows the value of combining diet changes with traditional treatments.
Other treatments being explored include anti-inflammatory drugs and supplements. Healthcare providers can create treatment plans based on what each patient needs. This way, they can get better results from the treatments.
Personalized treatment plans can do more than just manage symptoms. They can also prevent depression from becoming a long-term problem. By focusing on the individual, mental health care can truly make a difference in people’s lives.
| Treatment Type | Key Benefits | Considerations |
|---|---|---|
| Atypical Antidepressants (e.g., Esketamine) | Rapid symptom relief, especially for treatment-resistant cases | May require supervision, potential side effects |
| Probiotics | Improves mood and cognitive function | Longer-term studies needed for conclusive results |
| Dietary Interventions | Holistic approach that influences inflammation and gut health | Consistency is key; may require dietary changes |
Conclusion
Understanding how neurotransmitter imbalances connect to depression is key. The chance of facing Major Depressive Disorder (MDD) in a lifetime is 16.2%. In just one year, this goes down to 6.6%. It’s important to note that 73% of people with MDD will face it again. This shows why it’s crucial to focus on neurotransmitters when treating depression. Also, individuals with ongoing MDD episodes have only a 1% chance of getting better after five years. This highlights the struggle many endure with their mental health.
Treatment plans need to cover different strategies to help patients better. While 74% of those with MDD have it more than once, medication alone isn’t enough. Combining drugs with lifestyle changes, therapy, and support leads to better results. To keep improving treatments, ongoing research is necessary. This research helps us understand mental health better over time.
The debate on serotonin’s role in depression shows we must keep improving treatments. Looking into genetics and how poor sleep affects depression can improve treatments. The goal is a full approach that helps with recovery and overall well-being.