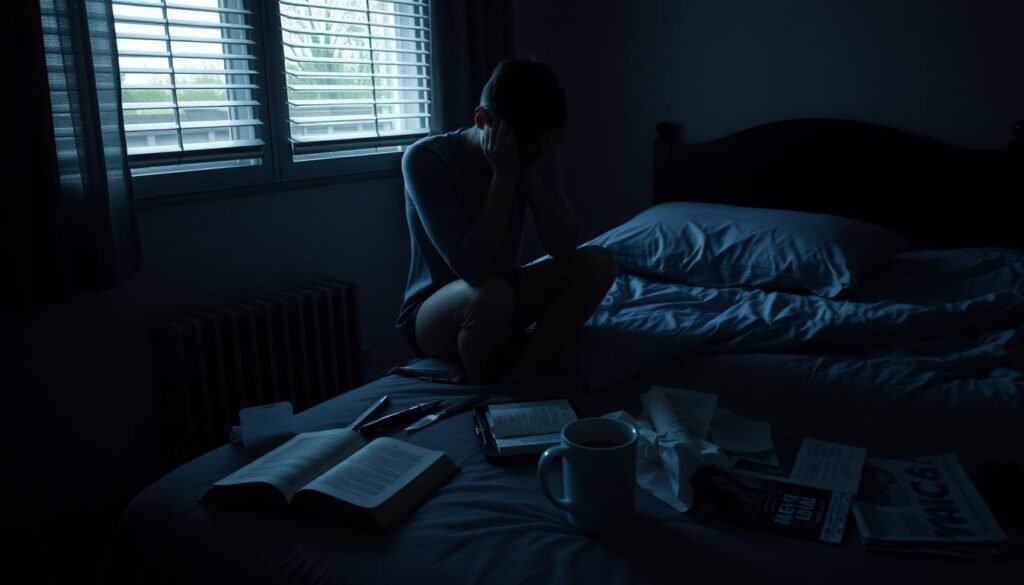
What if the ways you think are helping you stay mentally well are actually making you more likely to fall back into depression? It’s important to understand how to stop a relapse in depression. This is because many people think they are done once they start feeling better. But depression is a major cause of disability around the world, affecting about 18.4% of Americans every year. Since about half of all people will face depression again after their first time, and the risk grows with every relapse, we need to look at strong mental health strategies for lasting stability.
This guide offers expert advice on avoiding depression relapse, using research and practical steps. We will cover how to recognize symptoms and find out what triggers them. This article aims to show key preventive measures and therapies. Let’s start this path to better mental health together.
Key Takeaways
- Understanding the difference between relapse and recurrence can guide treatment.
- Preventing relapse in depression often involves a combination of therapy and medication.
- Regular self-care strategies contribute significantly to mental health stability.
- Social support systems play a vital role in preventing relapse.
- Identifying personal triggers is essential for effective relapse prevention.
- Mindfulness and cognitive-behavioral therapy approaches can help change negative thought patterns.
Understanding Relapse and Recurrence in Depression
Learning about depression includes knowing the difference between relapse and recurrence. It’s key to realize depression is a long-term issue. Relapse means symptoms come back quickly after getting a bit better, happening within six months of treatment. This is worrying because about half of the people with depression face relapse. This usually occurs in the critical six months after help like therapy.
Recurrence, however, is when depression comes back after being fully gone for six months. It’s less frequent than relapse but still very important for keeping mental health stable. Factors that might raise the risk of relapse include having had many depressive episodes, depression starting early in life, immune problems, and family history. Being a certain gender or age can also make relapse more likely, showing why treatments need to be personalized.
Sticking to the medication plan can greatly lower the chance of relapse in the crucial first six months. Using therapies like mindfulness can also help prevent relapse, especially for those who follow their treatment closely. This shows why it’s vital to actively manage mental health and for doctors to customize care for each patient.
| Aspect | Relapse | Recurrence |
|---|---|---|
| Definition | Return of symptoms within six months of partial remission | Onset of new episode after six months of complete recovery |
| Commonality | Occurs in approximately 50% of those affected | Less common than relapse |
| Impact of Treatment | Completion of medication reduces risk significantly | Requires ongoing engagement in treatment |
| Example of Management | Mindfulness and cognitive therapy | Personalized long-term strategies |
Symptoms of Depression Relapse
It’s important to know the signs of a depression relapse to help early. People may see signs they’ve had before and new ones. Key signs are:
- Persistent sadness
- Fatigue and low energy
- Changes in sleep patterns
- Alterations in appetite or weight
- Loss of interest in previously enjoyed activities
- Emotional numbness or detachment
- Physical discomfort or chronic pain
If these signs don’t go away after two weeks, depression might be coming back. Up to 60% of people with depression face relapses. Knowing these signs helps spot a relapse early. This means you can talk to health experts sooner to update your treatment plan.
Relapses are common in the first six months of starting treatment. Sticking to your full treatment plan is key. It might have therapy, medicine, and changes in your daily life to keep your mental health stable. Being aware and recognizing relapse signs means you can manage your mental health better.
| Symptom | Description | Duration for Concern |
|---|---|---|
| Persistent Sadness | A feeling of deep sorrow that does not fade. | More than 2 weeks |
| Fatigue | Constant tiredness that disrupts daily activities. | Ongoing for weeks |
| Sleep Changes | Insomnia or excessive sleeping. | Consistent over 2 weeks |
| Loss of Interest | Lack of enthusiasm for hobbies or social interactions. | Extended period |
| Emotional Numbness | Feeling detached from emotions or surroundings. | Lasting longer than 2 weeks |
| Chronic Pain | Physical aches not linked to other health conditions. | Persisting symptoms |
Identifying Triggers for Relapse
Understanding triggers for depression relapse is key to managing mental health. Triggers come from outside, like stressful events, and inside, through feelings. Knowing them helps people prevent relapse.
Common Triggers to Watch Out For
Some triggers for depression are:
- Life changes such as job loss or relationship issues
- Substance use, especially in people with past addictions
- Sleep problems that affect mood
- Untreated health issues impacting well-being
- Places linked to previous substance use
To avoid relapse, spotting these relapse triggers is crucial. For more details, you can read this article.
The Role of Stress in Relapse
Stress and depression often go hand in hand. High stress can make depression worse, leading to relapse. Stressful events can make one feel hopeless.
Key stressors include:
- Work stress
- Family arguments
- Money worries
Knowing the effect of stress helps in finding ways to cope. A good support system and mindfulness are important for mental health.
Preventing Relapse in Depression
To stop depression from coming back, it’s crucial to care for yourself in many ways. People with depression gain a lot from having a plan that keeps their mental health strong. It helps a lot to do regular things for your mental health. This means eating well, getting enough sleep, and staying active.
Importance of Self-Care
Self-care is key for staying mentally healthy. It lets people manage their health and fight off depression. Every day, small acts of care can make a big difference.
- Adhering to treatment plans as prescribed by healthcare professionals.
- Incorporating regular physical activity to boost mood and energy levels.
- Maintaining a balanced diet rich in fruits, vegetables, and whole grains.
- Prioritizing quality sleep to enhance emotional and cognitive functioning.
Through self-care, you can prevent depression from returning and boost your mood.
Key Lifestyle Changes to Implement
Changing your lifestyle can help a lot in fighting depression. These changes are important:
- Practicing mindfulness techniques to reduce stress and improve emotional regulation.
- Engaging in enjoyable hobbies and activities to foster a sense of fulfillment.
- Establishing regular routines to create stability and predictability in daily life.
- Maintaining regular contact with supportive friends and family members to strengthen social connections.
These changes can help keep depression away and make life more enjoyable.

| Lifestyle Change | Benefit |
|---|---|
| Regular Exercise | Boosts mood and reduces anxiety. |
| Healthy Diet | Provides essential nutrients for brain health. |
| Mindfulness Practice | Enhances emotional resilience and reduces stress. |
| Established Routines | Creates a sense of stability and normalcy. |
| Supportive Relationships | Offers emotional safety and encouragement. |
The Role of Medication in Relapse Prevention
Medication is key in preventing depression’s return and keeping stability. Knowing about different antidepressants aids in choosing the right treatment. Following doctors’ orders closely helps manage mental health and reduce the chance of depression coming back.
Types of Antidepressants for Maintenance Therapy
SSRIs and SNRIs are common antidepressants. They’re proven effective for ongoing treatment. A big study showed these drugs help prevent depression’s relapse much better than no treatment.
Taking these medications long-term is crucial. Those who keep taking their meds might not see depression return for about 40 months. Without medication, depression might come back in just over a year. This highlights the need to pick the proper drug and keep up with doctor visits for any changes.
Importance of Medication Adherence
Sticking to your medication plan is fundamental in treating depression. Not following the plan closely can risk depression returning. Healthcare providers warn against stopping meds too soon. They recommend continued use, tailored to meet individual needs. To stay on track, try reminders or support from loved ones.
Knowing how important medication is for depression and the options available helps individuals take control of their mental health. With continued help and observation, facing treatment challenges and avoiding relapse is possible.

| Antidepressant Type | Effectiveness in Relapse Prevention | Common Side Effects |
|---|---|---|
| SSRIs | High | Nausea, insomnia, sexual dysfunction |
| SNRIs | High | Dizziness, dry mouth, sweating |
| Tricyclic Antidepressants (TCAs) | Moderate | Weight gain, constipation, blurred vision |
| Monoamine Oxidase Inhibitors (MAOIs) | Moderate | Hypertensive crisis, dietary restrictions |
Cognitive-Behavioral Therapy as a Prevention Strategy
Cognitive-Behavioral Therapy (CBT) is crucial for preventing depression from coming back. It teaches people to identify and change negative thoughts. This helps develop better ways to cope. By adjusting how we think, CBT helps keep depression at bay.
CBT turns harmful thoughts into helpful ones. This promotes a tougher mindset. Strategies from CBT make a big difference in handling tough thoughts.
How CBT Helps Change Negative Thought Patterns
CBT works on thoughts, feelings, and actions. It helps people spot and fix unhelpful thinking. For many, CBT works better than usual treatments over time.
It stays effective even after sessions end. CBT reduces the chances of falling back into depression. Thus, it’s a top pick for fighting mental health issues.
Integrating CBT into Daily Life
Using CBT every day is important. Activities like writing in a journal and mindfulness help. They make the therapy’s effects stronger in real life.
This boosts emotional strength and lessens depression symptoms. Practicing CBT all the time helps handle stress and avoids depression’s return.
| CBT Techniques | Benefits |
|---|---|
| Cognitive Restructuring | Reduces negative thinking |
| Behavioral Activation | Increases engagement in positive activities |
| Mindfulness Practices | Improves present-moment awareness |
| Journaling | Facilitates emotional processing |
| Goal Setting | Enhances motivation and focus |
These strategies greatly lower the chance of falling back into depression. They show the value of sticking with CBT skills after therapy. For deeper insight into depression and coping methods, it’s wise to consult a professional. To learn more about managing mental wellbeing, click here.
The Benefits of Mindfulness Meditation
Mindfulness meditation is key for managing depression. It goes beyond just relaxing. It helps improve mental health in many ways. Practicing mindfulness regularly helps people control their feelings. It boosts self-awareness and brings peace to the mind.
Mindfulness Techniques to Reduce Relapse Risk
Using mindfulness daily can help prevent depression from coming back. Techniques like body scanning and mindful breathing help people reconnect with themselves calmly. These methods build resilience against stress and anxiety. Research shows that mindfulness-based cognitive therapy (MBCT) prevents depression as effectively as medication. It’s especially helpful for those who’ve had depression multiple times.
How Mindfulness Affects Mental Health
Mindfulness meditation positively changes mental health. It eases depression symptoms and reduces anxiety and stress. People in mindfulness programs often see big improvements in their mental health. This can lead to much lower chances of depression returning. While it may not replace medication for everyone, mindfulness helps treat depression and anxiety. For those interested, many studies on MBCT show its benefits.
Building Strong Social Support Systems
Creating a strong support network is key for those fighting depression. Research shows that this support leads to better treatment results, lower chances of falling back, and a happier life. Good relationships provide emotional aid, helping to reduce loneliness, offer coping methods, and increase toughness in tough times. It’s very important for anyone dealing with mental health issues to seek out relationships that encourage their recovery journey.
Importance of Relationships in Recovery
People with solid support circles tend to keep up their progress and reach long-term aims more easily. Studies link strong social ties to better results in avoiding a relapse. Emotional bonds also make it easier to share experiences and tips, helping to spot and manage stress triggers. Being part of support groups offers a safe place for talking about challenges, which boosts mental and emotional health. According to research, well-supported individuals are less likely to suffer repeated depression thanks to the grounding influence of these.
How to Seek and Offer Support
To build a helpful network for tackling depression, people should seek out family, friends, and group support. Peer support is crucial for recovery, offering understanding and hope through shared stories. Also, providing support to others can improve one’s own coping skills and make bonds stronger. By being open about personal struggles, an environment for mutual growth and healing through understanding and kindness is created.