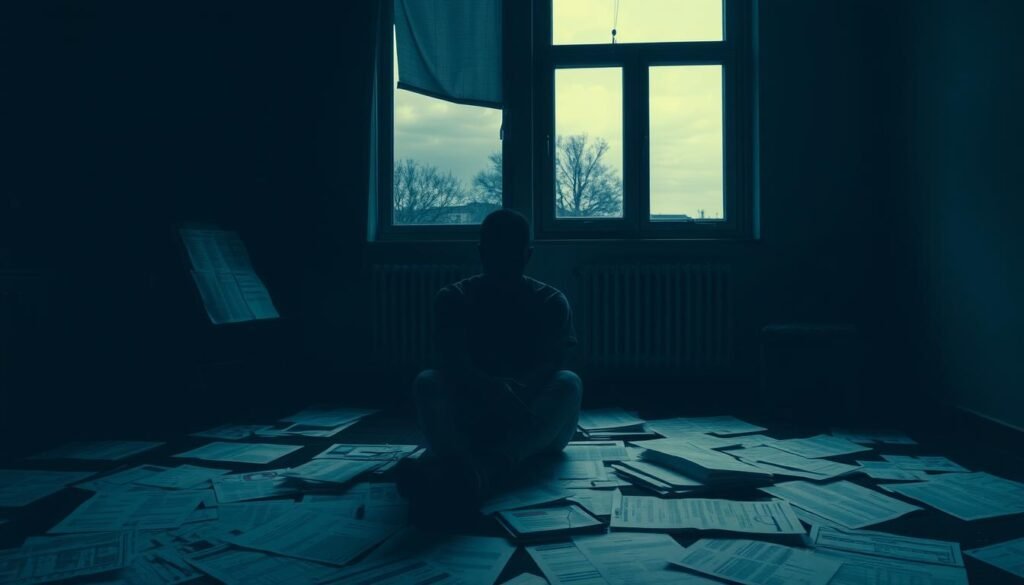
What if the sadness you see in others is more than a temporary mood? What if it’s a serious condition that often gets missed? Melancholic depression is a reality that challenges our views on mental health. Around 25% to 30% of people with major depression face this severe form. It is not easy to diagnose and treat because it has unique features. It is different from other types of depression, like dysthymia or chronic depression. This guide will give a detailed look at melancholic depression. We will cover its symptoms, risks, and how to manage it effectively.
Key Takeaways
- Melancholic depression significantly influences the central nervous system.
- Symptoms can surface later in life, often worsening in cold or low-sunlight seasons.
- Genetics and family history can increase the risk of developing this type of depression.
- Effective treatment options include tricyclic antidepressants and electroconvulsive therapy (ECT).
- Untreated melancholic depression can result in serious health complications.
What is Melancholic Depression?
Melancholic depression is a severe form of major depression. It comes with an intense sadness and a notable disinterest in activities. This type of depression has specific features that make it stand out from others. People with this condition often move, speak, and think slower.
The DSM-5 highlights melancholic traits as signs of severe depression. Those with melancholic depression might have more psychotic features. They also have a higher chance of needing hospital care and a greater suicide risk than those with other depressions. This highlights the seriousness of melancholic depression.
Older adults and inpatients are more likely to suffer from this condition. Studies show it has biological roots, with brain scans revealing unique markers. For treating melancholic depression, tricyclic antidepressants work better than SSRIs or therapy alone.
Melancholic depression deeply affects pleasure and interest in life. Those symptoms significantly impact work and social life. This stresses the importance of finding effective treatments and support.
For more details on melancholic depression and its implications, further exploration is encouraged.
Signs and Symptoms of Melancholic Depression
It’s vital to know the signs of melancholic depression for timely help. This condition has unique symptoms that impact life greatly. People with it are deeply sad and physically different from those with mild depression.
Loss of Interest in Daily Activities
One key sign is a big loss of interest or pleasure in fun activities. This is called anhedonia. It affects hobbies, friends, and daily duties. Folks struggle to do things they used to love, feeling lonely and helpless.
Physical Symptoms Associated with Melancholic Depression
Melancholic depression also shows physical signs. Common ones are:
- Significant weight changes or changes in appetite
- Sleep problems like insomnia or sleeping too much
- Always feeling tired or having no energy
- Having body aches and pains that won’t go away
- Being slow-moving or very restless
These physical issues are tough and can mix with feeling sad. About 70% of sufferers also have more health problems. That’s why looking at the whole picture is key. Recognizing these signs early helps start the right treatment sooner.

Causes and Risk Factors of Melancholic Depression
Several factors, including genes and environment, help us understand melancholic depression. People with a family history of mood issues are more likely to face melancholic depression. This serious form of depression affects how one feels, works, and interacts with others.
Genetics and Family History
Genes are key in melancholic depression. Out of six people, one will battle a major depressive episode in life. Those with family history face a greater risk. Health problems like diabetes and heart disease can also make depression more likely. Experiencing a lot of stress and having negative thoughts can make people with a family history of depression more vulnerable.
Age and Seasonal Changes
Getting older and the time of year can affect melancholic depression. It’s more common in older adults and gets worse in the cold, dark months. Brain chemistry changes, especially with serotonin, play a role. Big life changes, such as having a baby or going through menopause, can make people more prone to this type of depression. Knowing these risk factors is important for prevention and help.

| Factor | Description | Impact on Risk |
|---|---|---|
| Genetic Predisposition | Family history of mood disorders increases vulnerability. | High |
| Age | Onset is common in later life, linked to life transitions. | Moderate |
| Seasonal Changes | Symptoms often worsen in winter months due to less sunlight. | Moderate |
| Health Conditions | Diabetes, heart disease, and hormonal changes contribute to risk. | High |
| Stressful Life Events | Trauma and lack of social support elevate risk factors. | High |
Diagnosing Melancholic Depression
Qualified mental health professionals are needed to diagnose melancholic depression. They conduct detailed evaluations to identify key symptoms. To confirm melancholic depression, the DSM-5 criteria require one or both core symptoms. These are anhedonia or a deep loss of interest in enjoyable activities, plus three related features.
Such features could be significant weight loss, sleep issues, psychomotor changes, fatigue, guilt, or mood reactivity. Understanding these symptoms is vital. It greatly increases the accuracy in diagnosing this type of depression.
Recent studies, like the Sydney Melancholic Prototypic Index, have improved our ability to tell melancholic depression apart from other types. This method measures symptoms in a new way, capturing the true nature of melancholia more effectively.
Mental health experts also look at patients’ medical and family histories, as those with melancholic features often have a family history of depression. They also perform tests to check for other health issues that could affect mood. Their goal is to diagnose accurately, leading to the best treatment options.
New methods and research are constantly improving how we diagnose melancholic depression. Imaging studies show that people with this condition have less brain connectivity in certain areas. This is compared to those without depression and those with other depressive disorders. These findings help experts accurately identify melancholic depression, setting it apart from other mood disorders.
If you’re looking for more information, considering antidepressants as a treatment might be beneficial. This can offer more insights into handling symptoms of melancholia.
Treatment Options for Melancholic Depression
Treating melancholic depression needs careful planning. People with this kind of depression often get better results with certain treatments. The key treatments include medications, ECT, and psychotherapy. Each is chosen based on what the patient needs most.
Medications
Antidepressants are the go-to for melancholic depression. TCAs work especially well, more so than SSRIs, for this kind. Drugs like imipramine and amitriptyline are common choices. SSRIs are also options, giving patients more meds to try. Finding the right med or mix might take some testing. Blood tests can help figure out which antidepressants could work best.
Electroconvulsive Therapy (ECT)
If meds aren’t enough, ECT is another option. It helps correct the brain’s chemical balance and improve depression symptoms. Though ECT is sometimes seen in a negative light, it has been a lifeline for many with severe melancholic depression. The benefits it offers often surpass the short-term side effects.
Psychotherapy Approaches
Talk therapy plays a crucial role alongside meds and ECT. It helps by tackling harmful thought patterns and boosting coping strategies. It also delves into the patient’s relationships that feed into their depression. Depending on what suits the patient best, therapies like cognitive-behavioral or interpersonal may be recommended.
| Treatment Type | Description | Examples |
|---|---|---|
| Medications | Antidepressants used to balance neurotransmitters in the brain. | TCAs, SSRIs, SNRIs |
| Electroconvulsive Therapy (ECT) | Medical treatment that uses electrical stimulation to alleviate severe depression. | Used when medications are ineffective |
| Psychotherapy | Talk therapy to explore emotions, thoughts, and behaviors related to depression. | Cognitive-behavioral therapy, interpersonal therapy |
Combining treatments can really help those with melancholic depression. For more details on treating this condition, check out this professional health source.
Managing Melancholic Depression: Lifestyle Changes
Making big lifestyle changes is key to handling melancholic depression. These changes help ease symptoms and boost overall health. Adding physical activity, eating well, and sleeping enough are important. They help manage depression and improve mental health.
Exercise and Physical Activity
Regular exercise is a strong way to fight melancholic depression. Exercising for 30 minutes, 3 to 5 days a week, helps. It makes you more resilient to stress and improves your mood. Endorphins released during exercise play a big part. Activities like walking, running, or yoga are good for both mind and body.
Healthy Eating Habits
Eating right is crucial when dealing with melancholic depression. Foods rich in magnesium, folic acid, and vitamin B are good for your mood. A study showed eating branched-chain amino acids might lower depression risk. So, eating a balanced diet is an important step.
Establishing a Sleep Routine
Good sleep matters a lot for mood regulation. People with melancholic depression often struggle with sleep. This can make fatigue and depression worse. Setting up a regular bedtime schedule helps improve sleep. Practices like meditation can enhance sleep quality and lower depression-related anxiety.
Complications of Untreated Melancholic Depression
Untreated melancholic depression goes beyond feeling sad. It affects both your body and mind. Knowing these issues is key for those suffering and for doctors trying to help.
Physical Health Issues
Not treating depression can lead to serious health problems. People might face:
- Substantial weight loss, leading to malnutrition.
- Chronic pain, linked to mood disorders.
- Increased risk of heart issues, affecting long-term health.
A lot of research shows the connection between melancholic depression and physical health troubles. For deeper understanding, check out this study on mental health outcomes.
Impact on Relationships and Daily Life
The weight of melancholic depression also hurts personal relationships and everyday life. It can cause:
- Problems with family and friends, due to pulling away or getting easily upset.
- Poor performance at work, which might lead to losing a job or stalled career.
- Avoiding social activities, making one feel lonely.
Understanding these issues helps in seeking early help. This is crucial for better mental health. It’s important to deal with these problems to improve life and relationships.
Conclusion
Understanding melancholic depression is essential for everyone involved. This type of depression is not new. It was common in British asylums by the late 1800s. Back then, a lot of people with this condition sadly thought about suicide often. This shows why it’s so important to know the signs and how to help.
Treatments can really make a difference in people’s lives. Nowadays, we connect melancholia with other depression types. Knowing this can lead to better help and support for those in need. Everyone should know that things can get better with the right diagnosis and help.
Dealing with melancholic depression takes a lot of work. It requires learning, understanding, and action from both the person affected and their supporters. By working together and staying hopeful, they can face this challenge. This effort brings hope and strength to everyone involved.